What Is The Hemispherectomy?
A hemispherectomy is usually performed on young children, as neuroplasticity is better at a young age and the healthy half of the brain can take over various functions of the distant part of the brain.
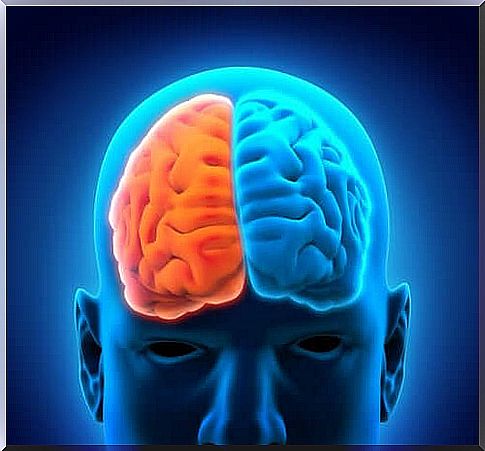
A hemispherectomy (brain amputation) is the neurosurgical removal of one half of the brain. It is intended to treat severe cases of epilepsy with uncontrollable cramps in one hemisphere. This operation is only carried out if all other options have already been exhausted without success.
It is believed that the first hemispherectomy was performed in 1888. The first human references to this procedure date back to 1923. Several operations of this type were performed in the 1960s and 1970s. However, these were not very successful.
In the meantime, the conventional hemispherectomy is often being replaced by a functional one. This type of intervention is more precise and less invasive. Therefore, the chances of success are much higher than in the past.
What is a hemispherectomy?
As mentioned earlier, this is a neurosurgical procedure that involves removing half of the brain. This type of intervention is mostly done in children between the ages of 5 and 10. This is to prevent strong donut attacks, which are usually triggered by epilepsy. However, a hemispherectomy can also be performed in patients with neurological damage and, in exceptional cases, in severe traumatic brain injury.
Usually an entire hemisphere is removed, but in some cases only a specific area of the brain can be amputated. In this case it is called a functional hemispherectomy. But if even a small part of the damaged tissue remains, cramps can recur.
When is a hemispherectomy considered?
This intervention is an option when patients are continuous; that means practically every day suffering from intense cramps that could not be relieved pharmacologically or by other, less invasive surgical interventions.
A hemispherectomy can be considered in the following cases:
- Hemiplegia in children. When children over 4 years of age have convulsive seizures that last for 2 years and cannot be relieved by pharmacological treatments.
- Sturge Weber Syndrome. This is a rare neurocutaneous disorder characterized by malformed capillaries on the face or cerebral and ocular vascular malformations. Affected children can suffer from epileptic seizures, among other things. A hemispherectomy is an option if the seizures start at a young age and affect an entire hemisphere of the brain.
- Rasmussen’s Syndrome. This is a progressive inflammation of certain areas of the cerebral cortex. In this case it is advisable to intervene as early as possible.
- Hemimegalencephaly. This is a neurological inflammatory disease that occurs very rarely and is characterized by severe seizures. Whether or not a hemispherectomy is useful in this case is still open to debate.
- Variations in cortical development. If there is unilateral brain damage in one hemisphere, a brain amputation can be considered.
Various options for intervention
There are four different ways to carry out this intervention, the success of which depends fundamentally on the hemostasis (hemostasis):
- Anatomical hemispherectomy
- Hemidecortication
- Functional hemispherectomy
- Modified functional hemispherectomy
General anesthesia is usually required for this procedure. After shaving the head, the surgeon marks the incision sites. This is followed by the surgical opening of the skull. The dura mater (outermost meninges) is removed to gain access to the brain. The neurosurgeon then marks the area to be removed and begins the brain amputation. After removal, the blood vessels must be cauterized and drainage is also necessary.
The surgeon then closes the opening and secures the skull bones with clamps.
After the hemispherectomy
The recovery phase is very painful. The drain is usually removed after 3 to 4 days, as assessed. Before doing this, however, diagnostic tests must be done to see if there is any bleeding.
The most common immediate complications are associated with unstable hemodynamics, hypothermia, and hypo- or hyperkalemia. The patient is usually in the intensive care unit during this time.
If cramping occurs in the first stage after surgery, it is a serious complication. About half of the patients have hydrocephalus (head of water) and almost all sufferers develop aseptic meningitis. The death rate is between 4 and 6%.
70 to 85% of patients can control seizures after the intervention. Between 10 and 20% can significantly improve their quality of life. It should not be forgotten that certain complications can only arise much later.